New Beginnings
This toolkit gives a step-by-step guide for using the experience based co-design (EBCD) method for maternity services based on the ‘New Beginnings’ Project led by Emma Evans, Consultant Anaesthetist, Andrew Tan, Anaesthetist, and Julia Crawshaw, Programme Manager for Maternity Transformation at St George’s University Hospitals NHS Foundation Trust. It focused on the experience of women who give birth in the operating theatre or have part of their birthing experience there, and the staff who work in theatre.
Thanks to all those who took part in the project and supported it, and helped in the production of this toolkit. This project was funded by the Health Innovation Network South London https://healthinnovationnetwork.com/
Listen to Andrew describe why they wanted to improve the experience in the operating theatre through the launch of the New Beginnings project.
Background
Although only one in four women give birth in theatre, 40% have some part of their experience in the theatre. It has been shown that mothers experiencing operative delivery have a poorer care experience than women having non-operative deliveries. These women often find themselves falling outside the ‘normal’ agenda in birth experience discussions and planning, particularly if the decision to deliver operatively has been made late in pregnancy or in labour.
Maternity theatres can also be an area of poor staff experience, with operating department staff often feeling somewhat isolated from the rest of the maternity department. This leads to lack of ownership and empowerment to develop practices around patient or staff experience.
Emma Evans, a consultant anaesthetist at St George’s University Hospitals NHS Foundation Trust, was keen to ensure mothers’ “first moments with their babies were amazing.” Emma had attended the Point of Care Foundation’s EBCD training and thought the method would be ideally suited to improving the experience of women who had some part of their birth experience in the operating theatre.
In 2018, Dr Emma Evans (consultant anaesthetist), Dr Andrew Tan (consultant anaesthetist), Julia Crawshaw (Programme Manager, Maternity Transformation) at St George’s initiated the New Beginnings project which gathered staff views and women’s views using filmed interviews. Co-design events were then held to decide which were the most important themes to work on.
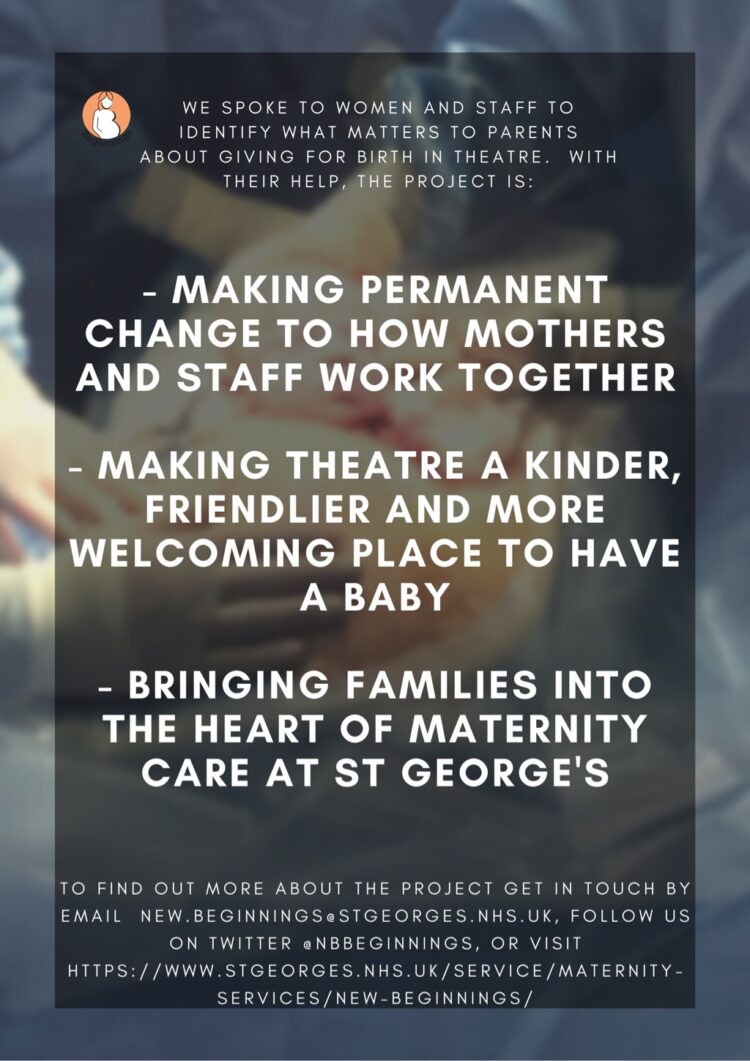
New Beginnings’ aims were:
- To develop a patient-centred approach to the way operative delivery care pathways were designed and delivered.
- To give patients a voice over and above traditional forums for patients (which don’t often represent those outside normality).
- To create greater value to the contribution of team members to the environment in which they work, with a view to impacting on their performance, including attitudes and behaviours and their confidence to design and implement organisational change.
Patient experience
New Beginnings made changes that meant the process of “normal” birth was mirrored as far as possible in the theatre. This included things such as, choices in the environment, or how the parents discovered the sex of their baby. It meant greater sensitivity to the dignity of women on their way to theatre and once inside the theatre.
There were changes to the clinical processes because of the project also. For example, reviewing the length of time the women were “nil by mouth”, having heard the story from one mother who had been without fluids for many hours on one of the hottest days of the summer. “I was crying, and it sounds stupid now, I was so thirsty I tried to drink my tears.”
The families described eloquently how finding themselves in theatre often came as a shock, and they found they were in a “surgical” experience rather than a “maternity” experience. This meant that a lot of things people prepare for when writing their birth plan can get overlooked.
Staff experience
St George’s maternity staff who were involved in New Beginnings identified a whole range of process improvements that they thought would benefit both parents and the staff. For example, how to organise the care pathway to enable the maximum possible continuity of care between the midwife and the family. They wanted to improve handovers, and the environment which affected families as well as staff.
A finding that had a big impact on the staff was seeing the impact seemingly innocuous clinical processes had on the mothers. One mother (whose baby was being checked over just out of sight) described how, “no-one was saying anything. It was probably only one or two minutes, but for those few minutes, I thought he’d died.”