Making healthcare more human: Patient perspectives
18 April 2018
Bev Fitzsimons looks back at what we learned about patient experience at last month’s conference on ‘Making Healthcare More Human’.
Topics
At our recent spring conference, the theme was ‘making healthcare more human’ – or more specifically, what it means to be a patient, what it means to deliver care, the relationships between carers and the cared for, and what each brings to the other. Why this theme? The emergence over a number of years of evidence about the absence of humanity in the system for both staff and patients.
What was unique about the conference was the sense of equality in pursuit of a common aim between staff and patients: easily more than half of the speakers came with a ‘patient hat’ on, although they all brought more than this. What was also unique was that sponsorship meant that many more people than usual who would not normally get to attend a conference were able to do so. This meant patients and patient leaders and junior staff from all professions, as well as the more senior ‘usual suspects’. It felt as if we were listening to the future, rather than only the present and the past.
Empowering patients
Ceinwen Giles (a Point of Care Foundation trustee and Director of Shine Cancer Support) opened proceedings in conversation with a panel of patients. They brought with them (in her words) ‘a cornucopia of diseases’ – said in jest but reflecting the reality of what it means to be an ‘involved’ patient: reduced to a condition or disease, instead of reflecting on the assets they bring. If I re-wrote the sentence describing our ‘panel of patients’, I could describe them instead as a former head teacher, an international development worker and a doctor, all of whom are involved with health services and who can bring powerful insights from all of their experiences. Why, as a system, do we fail to make use of their insights?
For our panel members themselves, there is also a dilemma. When is a patient not a patient? Some people want to be identified as a patient, some don’t, and some do some of the time. As Tessa Richards (BMJ patient editor and doctor) said, ‘I still think I’m a patient, but a person first’. Equally, our panel reflected on their own impact on the staff looking after them (who are also ‘people first’). Rhiannon Flood, who survived cancer, courageously described her loss of self-esteem, anger and unhappiness following her treatment. ‘You don’t get great communication back when you put that out’, she said.
Healthcare professionals don’t go to work to do a bad job. So how is it that we hear again and again of exchanges that are transactional and seemingly without care? In part because illness and injury render you powerless, powerfully illustrated by Tessa describing being told to ‘pipe down’ when calling out in pain during treatment. And in part because it is difficult to put the patient at the centre of care when the system we work within does not.
‘It’s the system stupid!’ Tessa nailed it in identifying what gets in the way of humanity in healthcare, questioning how much value the system places on compassion and kindness. On Twitter meanwhile, the debate raged: on the one hand ‘surely fabulous healthcare professionals exercise autonomy in the behaviours they choose’. On the other ‘others blame the system’. Surely it’s a bit of both.
Staff-patient interaction
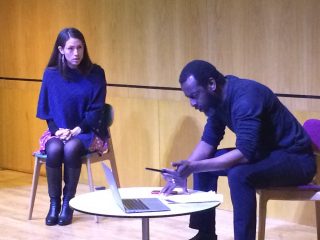
In our quest to deliver a different sort of conference, forum theatre group Performing Medicine enacted a scenario which was based on conversations with patients in advance. We saw a doctor-patient consultation in which the actors accepted challenges from the audience on how to make the consultation ‘more human’.
The issues illustrated are familiar, including professionals being busy and distracted; patients and staff feeling rushed; system failures meaning the right information is not in the right place for the right person at the right time; and both sides not feeling listened to. What is probably less familiar were the feelings of vulnerability on the part of both staff and patients. Although people have a pretty good idea of what ‘more human’ healthcare is, this doesn’t always translate into health professionals’ behaviours and practices in the heat of the moment.
The conversation in the coffee break afterwards was fascinating, with some discomfort with what was observed. ‘Could that be me? It couldn’t be me’. One of our patient panel members said, ‘It’s like half the consultations I’ve had – and not in a good way’. Whilst funny and exaggerated, there was general agreement that there is still evidence of this sort of practice. One doctor who is also a patient, in relation to the lack of time and notes described the performance as ‘amusing if it were not too often the norm’.
Patient experience professionals
The final session of the morning brought together patient leaders and professionals to reflect on the question of how to strengthen the relationships between patients and professionals, enhancing the humanity of the interaction for both. The fundamental starting point was remembering the purpose of healthcare: to serve the needs of patients and ease suffering. In which case, it is unquestionable that patients need to be involved at the most fundamental level. As David Gilbert, patient director at the MSK partnership in Sussex, said: ‘You wouldn’t want to provide a service for women that was run only by men’.
The conversation returned to the theme from earlier in the day, that people are more complex than their conditions, and they are often keen to ‘give back’ to the system. Lesley Preece, a patient partner at the MSK partnership, said: ‘I wanted to do something to help others so no one else would ever have to go through what I did’.
However, to be meaningful, efforts to truly share power with patients have to be authentic, and at every level from the strategic to the straightforward and practical. Patients’ entire experiences need to be valued, rather than their healthcare experience gathered as ‘feedback fodder’. Shared, collaborative decisions need to be in the DNA of organisational culture. You can’t expect it to happen in isolation at the front line.
When the system gets this right, it can have a profound impact on both staff and patients. David gave us an example from the MSK partnership in Sussex. By switching their process from one in which the system allocates people to appointments, to one in which people make appointments to suit demands on their time, vastly reduced the time spent dealing with appointment queries, as well as reducing the number of people not attending appointments. A simple example of a transfer of power from systems to people.
None of it is quick or easy, with David Gilbert describing ‘a really messy embarrassing awkwardness’ in bringing clinicians and patients together. But from what we heard from our panellists and audience, the benefits are immense in delivering a more human system for everyone.